Dr. Soh's radio interview
Dr. Soh discusses migraine and weather changes on 1110 KFAB weekend news radio.
David Nabity: I saw an article in the Omaha Herald that talked about a study linking extreme heat to migraine headaches. Evidently, the University of Cincinnati did a study that basically says that when weather changes and gets hotter, people have more migraine headaches.
Are people really getting migraine headaches as temperature goes up?
Dr. Soh: Migraine headaches are associated with many different factors. It could be genetics, it could be due to environment, to diet, sleep disruption, stress, and in the literature there is some data that shows that fluctuations in temperature, humidity can be a trigger for headache or migraine headache. However, there's multiple things that could happen at once that that could trigger a migraine headache.…So this study was based off diary data from about six hundred patients, and they tracked headache along with the different changes in weather in their regions, and they noticed that every ten degree change in temperature, there was an increased number of headache days. And this is approximately over a twenty-eight week period…it's really that change in temperature, that daily change in temperature.
David Nabity: Tell me what is a migraine headache?
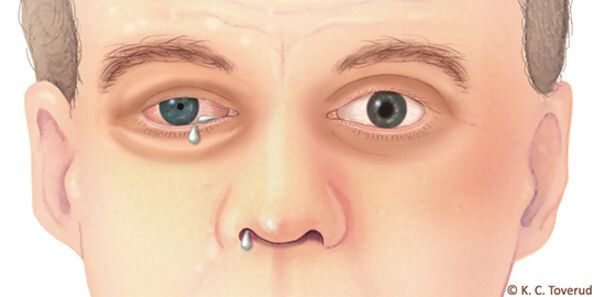
Dr. Soh: A migraine headache is a headache that by criteria is four to seventy-two hours that's either untreated or treated unsuccessfully. It'll have two of the following four characteristics (1) one-sided unilateral, (2) moderate to severe intensity, (3) throbbing, pulsating pain, and (4) pain worsened by movement. And at least one of the following two: (1) Light and sound sensitivity and/or (2) nausea and/or vomiting.
David Nabity: What I thought the article was saying is is hotter climates could create it more. But you're saying what they're saying is that if you're used to normal temperature pattern and then that temperature pattern increases no matter where. You could be in Alaska and you're used to thirty degrees right and then it goes to fifty, that could trigger it?
Dr. Soh: So the study looked at barometric pressure changes, dry bulb temperature, humidity, relative humidity. So these are all things that you want to look at more into detail. But this is just a kind of a correlation they're seeing, and there's no data to say that being in a hot temperature consistently worsens headache disorders. Clinically, what I see in practice, patients who are exposed to cold temperatures can be a trigger, so we got to look at both extremes. And I think the study is looking at the changes in temperature, but the news article may have not been stating it that way. So that's my interpretation.
David Nabity: Well, what do you do for somebody that has migraine headaches?
Dr. Soh: Well, migraine headaches they can either be very debilitating a few times a month or up to thirty days a month. So it depends on first of all, is the diagnosis correct? Is this patient really having a migraine headache? And if they're not, we got to think about secondary causes or headache disorders. And there are other disease processes that could be manifesting themselves as a headache disorder; like a brain tumor, vascular abnormality, infection, autoimmune causes, hormone imbalances, and metabolic disturbances.
David Nabity: Lime disease?
Dr. Soh: Yes, lime disease can have a symptom of headache. So I think seeing your physician or your health care provider if you're having headaches that are preventing you from going to work, preventing you from being social, keeping you inside the house, that's when you need to talk to a doctor or health care provider. Now, what do we do after we make the diagnosis correctly. Because it's a clinical diagnosis, there's no brain imaging, no blood work to say, ‘hey, you have a migraine disorder.’ This is all clinical through extensive history. To rule out the secondary causes, we might use lab work, you might use imaging and other tests, but once we have that ruled out, then we think about your clinical history. We make the diagnosis based off the criteria I had mentioned. And if you do have migraine, there can be chronic migraine, which is fifteen or more headache days a month, or episodic which is less than fifteen. And there's different treatments for that. There's medications, there's vitamins, there's lifestyle changes and other things that we can do to address the headache.
Co-host (Peter): So I'm also curious too, and I've always wondered this. So I've heard migraines can come from all ranges of things, from brain tumors and stuff that are mortally, a very serious disease physically but also mentally. How much or how many migraines would you say, or maybe a percentage of it as a result of physical malady? And maybe it's similar to that, or it's a mental stress or mental health or something like that.
Dr. Soh: So, just to clarify, migraine is a neurological disorder of the brain. It's a primary headache disorder. So the brain can get hyperactive, the vessels, the nerves that supply the vessels can get sensitive, and that's really coming from the brain itself. A headache due to a tumor would be a secondary headache cause so that would not be a migraine headache. And actually, in chronic migraine, up to fifty percent of patients have depression and or anxiety and so stress is a big trigger. And so that's why I was making the analogy.
Co-host (Peter): So what sort of drugs do you give people that have migraine headaches?
Dr. Soh: I first like to make the diagnosis and then ask patients what their goals are and expectations, and depending on how chronic or severe their headaches, I give them options based off their lifestyle, their preferences, and their medical needs.
Co-host (Peter): Well Tylenol is not going to do anything for it, right?
Dr. Soh: Actually, Tylenol one thousand milligrams. I'm not saying that this is for every patient, but that can be used for acute relief.
David Nabity: What do you get if you take two Tylenol? That's a thousand milligrams?
Dr. Soh: Right, doubles five hundred milligrams each. Five hundred milligrams is extra strength Tylenol.
David Nabity: So two of those can be - I didn't realize that. I thought it was one hundred milligrams. I would just do that weak stuff then.
Dr. Soh: But you know, talking to your primary care doctor or your physician really is the best thing to do when you're trying to treat your headache especially if they're debilitating. And that's what I would recommend first. The unfortunate thing is we don't have enough specialists out there or providers to treat patients because migraine headache effects twelve percent of the population. So that's approximately thirty nine million people in the US.
David Nabity: Wow. How much of that can just be caused by your neck being out of alignment and needing a chiropractic adjustment?
Dr. Soh: There can be myofascial components to headache, being the muscles get tight. There can be some neck disease in the spine that could be related to…
David Nabity: Yes, yeah, and when you say neck disease, what do you mean?
Dr. Soh: So disease in the cervical spine or muscles that are tight in the neck that can be a trigger for headaches. And there can be what they call a cervicogenic component. So it's actually a very complex problem that is a brain issue. But because there's a lot of pain sensory
fibers that are going around the face, the neck, the muscles, this can be linked to the headache disorder and make the symptoms worse or manifest its symptoms as being pain in that area, even though the pain is actually a brain disorder and the brain has no pain receptors inside the brain, but the covering of the brain around the vessels, those are the pain receptors.
David Nabity: I'm really curious as to your perspective in your opinion on chiropractic as a treatment for migraine? Do you think you can help or is that more of a no-no for you?
Dr. Soh: I get a lot of questions about that. There's not really a standard treatment for chiropractors. And one thing I say to patients when they do get care from chiropractors, I just say let's avoid any sudden movements of the head or neck because that sudden movement going left and right can cause a vessel dissection. The studies don't show a high incidence, but it is a possibility, and I don't have good data to say that chiropractor is actually helpful for treating headaches. Some patients do get relief from the chiropractor treatment in a safe manner, and because it's not standardized, I just give them the warnings and let them know, ‘Hey, if you're doing it, just be careful of this.’
David Nabity: So I noticed you brought this article about Caitlin Clark, the basketball star and she deals with migraines all the time, I guess.
Dr. Soh: And this is great because you know when celebrities and celebrity athletes who have migraine and let the media know, it reduces the stigma because migraine is an invisible disease.
David Nabity: And it's probably embarrassing, right for somebody to keep saying, I got a headache again, I got a headache again, headache again?
Dr. Soh: And this is why education is important for the public, so that this is a real disease that's disabling. And Caitlin Clark almost had a triple double apparently, I think she missed it by one rebound. In her postgame interview, she mentioned she has migraine and the lights and sounds from the stadium obviously makes it worse. And then during the game her adrenaline kind of helps her out, but after the game it just it's really impacts her negatively, but she plays through it.
David Nabity: This is just nice that you have a superstar athlete who can say, look, I'm dealing with migraine and people get more of awareness and maybe more comfortable with the diagnosis. How about how about little ones? You know, a mommy and a daddy can have a baby and there's this crying all the time. How do you figure out whether a little baby has migraine?
Dr. Soh: So that's a great question. There's actually headache specialists who are pediatric headache specialists. They go through different training than adult headache specialists. Patients can have headache before they are even talking. And a lot of patients I have will have headaches since they're as early as they can remember. And I think Caitlin Clark also mentioned she grew up with headaches growing up from younger to older. So it affects all populations, all ages. Economically, it's a huge impact. The huge population it affects is women more so than men, about three to one ratio, and usually that twenty to forties age range, when that's a very productive age range
in terms of work and raising families. So you could see the huge impact it has on not just quality of life, but economic impact. When we're missing a day of work or a social activity, it's a big toll on society and it's actually number two in disability in the world, behind low back pain, and that's measured in disability adjusted life years.
Co-host (Peter): So man, I'm so glad we talked a little bit about Tylenol, but besides that, what kind of treatment plans can you offer? And the research I'm sure it's an ongoing thing. It's a science. It's always evolving and developing stuff. So what are you looking at in helping these people who have suffered since childhood or maybe just recently developing this.
Dr. Soh: Thanks for circling back, Peter. The medications can range from vitamins like magnesium, riboflavin and, CoQ10. There can be preventive therapies if you're trying to prevent the headache attack…
Co-host (Peter): And these supplements can actually make a difference in this?
Dr. Soh: Yeah, the studies have looked at magnesium and three hundred eighty milligrams a day. I usually recommend four hundred to eight hundred milligrams nightly. And this is making sure this is done in a safe way that patients have no adverse side effects. But those can help with migraine. We have medications that were made for other conditions like high blood pressure, seizures, depression, and the mechanism of action actually helps with migraine headache. This is before the new medications came out. So even though I prescribe medication that's a seizure medication, it doesn't mean I think the patient has seizures, but that mechanism of action can actually help with the actual migraine headache. Then we have newer medications that came out over the last four to six years, and these block a molecule called CGRP. CGRP stands for calcitonin gene related peptide, and it's been found that this can be elevated in headache attacks. And so these new generation medications that are either injectable or by pill they can actually help reduce their frequency of headache attacks or treat acutely. And so there's not really one right therapy. Each patient is different.
David Nabity: You have to custom design it. Well listen, Peter, how can people get a hold of you?
Dr. Soh: The best way right now is going on the website, sohheadachecenter.com. They can read about the services we provide, read about if this is right for them, and then make an appointment through the website.
David Nabity: All right, well, listen, I appreciate you being here this morning. I'm sure there's somebody listening and like, ‘you know what that's got to be what I have and I need to do something about it.’ So I appreciate you being here.
Dr. Soh: I appreciate it really much.
David Nabity: All Right, we're going to take a break.